Contact us
Need more information? Your local key account manager will be in contact shortly.
This page is intended for UK healthcare professionals and other relevant decision makers only. If you are a member of the public, please click here.
This portal is funded and owned by Novartis Pharmaceuticals UK Ltd and includes content approved by Novartis.
Adverse events reporting information can be found in the footer of this page.
KESIMPTA is indicated for the treatment of adult patients with relapsing forms of multiple sclerosis with active disease defined by clinical or imaging features.1
For full safety information, please refer to the KESIMPTA Summary of Product Characteristics (SmPC).1
KESIMPTA has demonstrated efficacy in ASCLEPIOS I and II (2-year core studies), two Phase III randomised, double-blind, double-dummy, active comparator-controlled, parallel-group, multicentre pivotal trials, comparing a range of outcomes to active comparator teriflunomide in 1882 patients with relapsing MS, following patients for up to 6 years (including the 4-year extension phase, ALITHIOS study).1–3 ALITHIOS is an ongoing, open-label, single-arm, umbrella-extension, Phase IIIb study assessing the risk–benefit profile of KESIMPTA (20 mg subcutaneously every 4 weeks) and its tolerability in patients with RMS. The study enrolled 1703 patients with RMS from the APLIOS, APOLITOS and ASCLEPIOS I/II trials who continued KESIMPTA treatment.2,4 The primary endpoint, annualised relapse rate, was defined as the number of confirmed relapses of multiple sclerosis per year, according to pre-specified criteria. Secondary endpoints included disability worsening confirmed at 3 months and 6 months, disability improvement confirmed at 6 months, the number of gadolinium-enhancing lesions per T1-weighted magnetic resonance imaging (MRI) scan, the annualised rate of new or enlarging lesions on T2-weighted MRI, serum neurofilament light chain levels at month 3, and change in brain volume.3
KESIMPTA met the primary endpoint in ASCLEPIOS I/II, with up to 58% reduction in ARR vs teriflunomide (ASCLEPIOS I: 51% [0.11 vs 0.22]; RR: 0.49 [95% CI: 0.37–0.65]; ASCLEPIOS II: 58% [0.10 vs 0.25]; RR: 0.42 [95% CI: 0.31–0.56]; both p<0.001).3 Read more about the study designs here.
Click on the tabs below to find out the results for specific efficacy outcome measures.
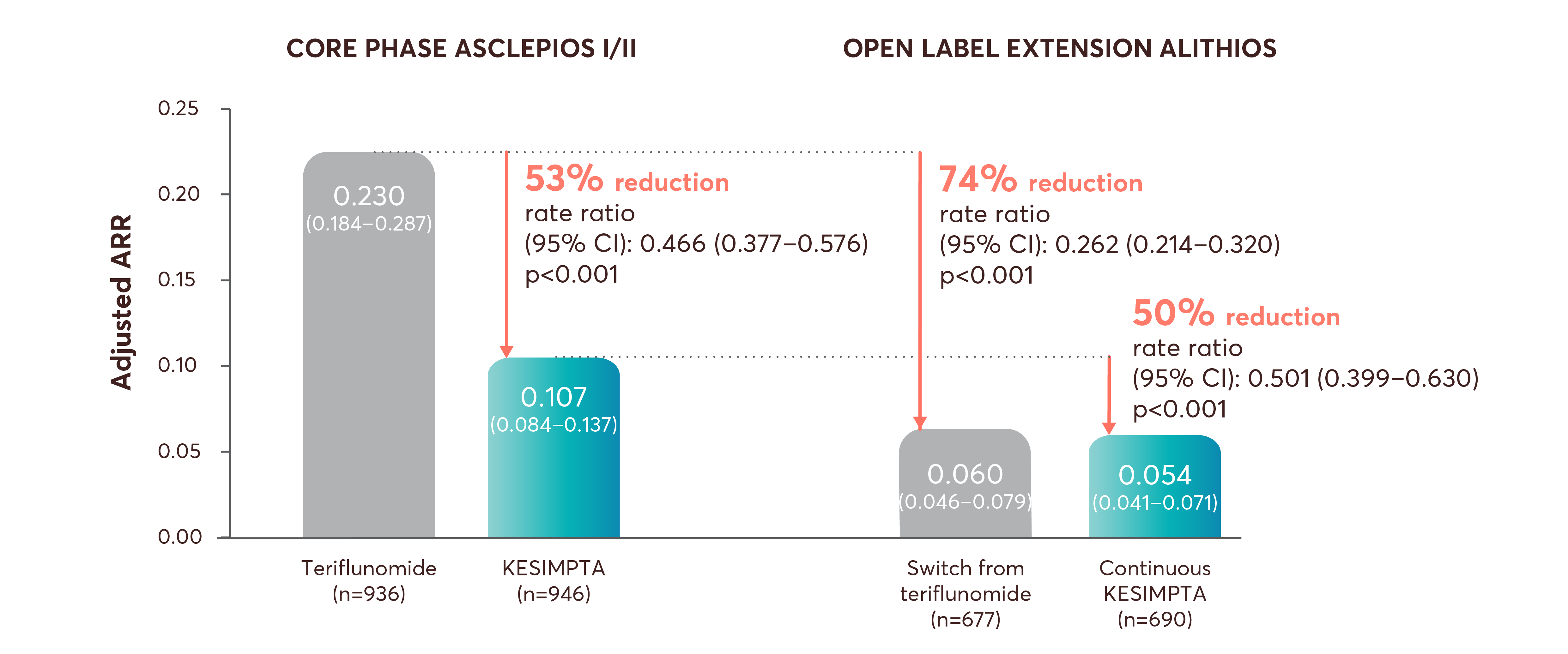
A low ARR was observed in participants receiving KESIMPTA for up to 6 years (data cut off: 25th September 2023)*2
ARR data at Year 6 – continuous KESIMPTA: ARR: 0.054 (95% CI: 0.041–0.071) [n=690]; teriflunomide–switch to KESIMPTA: ARR: 0.060 (95% CI: 0.046–0.079) [n=677]; p=0.416 (nominal p value).2
Within- and between-group comparisons during the core and extension phases for ASCLEPIOS and ALITHIOS†2
Adapted from Wiendl H, et al. 2024.2
The difference between the switch from teriflunomide and continuous KESIMPTA group ARR (0.060 vs 0.054) during the open-label extension phase was not statistically significant (10.8% reduction; RR [95% CI]: 0.892 [0.677–1.175]; p=0.416).2
A significant reduction in the ARR was observed for KESIMPTA versus teriflunomide in the core ASCLEPIOS I/II studies, and both groups receiving KESIMPTA in the extension study maintained a low ARR.2
At Year 6, 90% of KESIMPTA-treated patients achieved NEDA-3§2
NEDA-3§ (post-hoc analysis) at Year 6 – continuous KESIMPTA: 91.9% of patients achieved NEDA-3 (n=655); teriflunomide–KESIMPTA: 91.2% of patients achieved NEDA-3 (n=599); p=0.599 (nominal p value).2
Adapted from Wiendl H, et al. 2024.2
No evidence of disease activity (NEDA-3) was determined in a post-hoc analysis of pooled ASCLEPIOS trials.2,5,6
6-month CDW
Confirmed relapse
Gd+ T1 lesions AND new or enlarging T2 lesions
Adapted from Wiendl H, et al. 2024.2
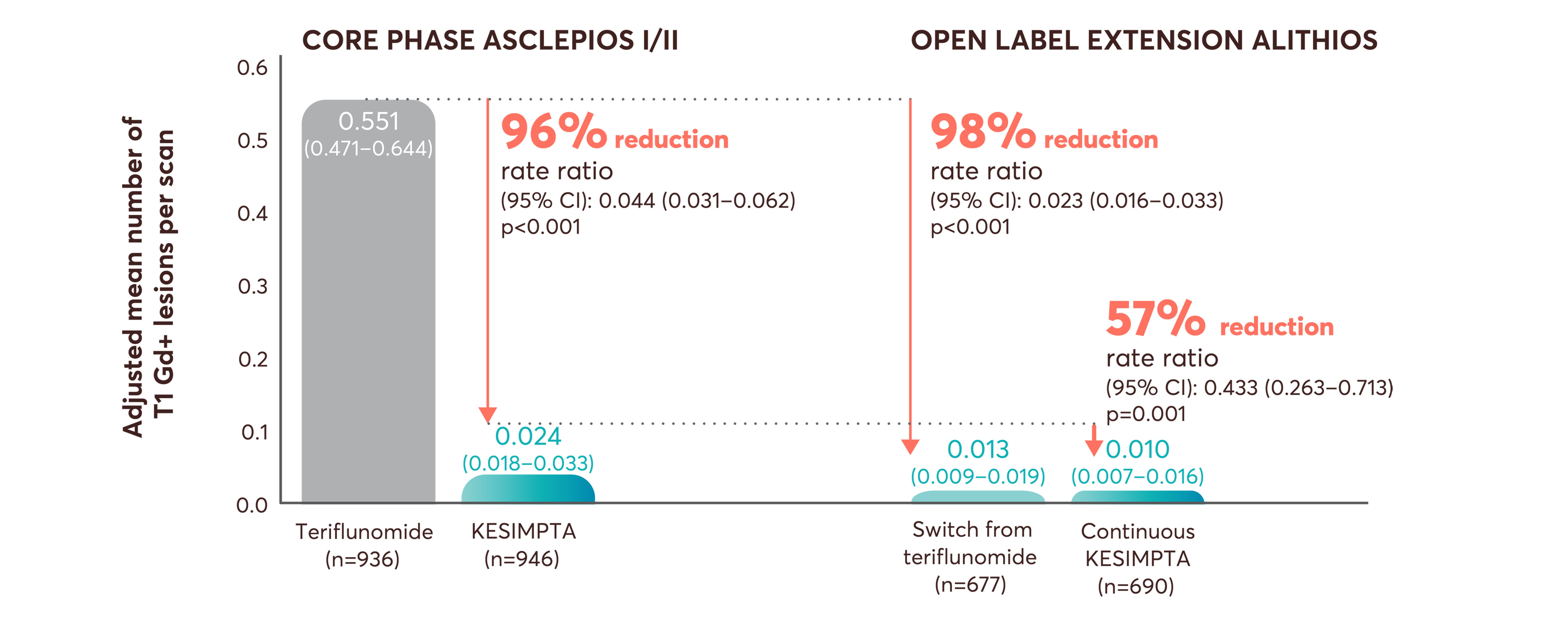
A significant reduction (95.6%) in the mean number of Gd+ T1 lesions was observed for KESIMPTA versus teriflunomide in the core ASCLEPIOS I/II studies. Gd+ T1 lesions were almost completely suppressed during the extension phase (ALITHIOS) in both the continuous KESIMPTA group and the switch group.2
Within- and between-group comparisons during the core and extension phases for ASCLEPIOS and ALITHIOS¶2
Adapted from Wiendl H, et al. 2024.2
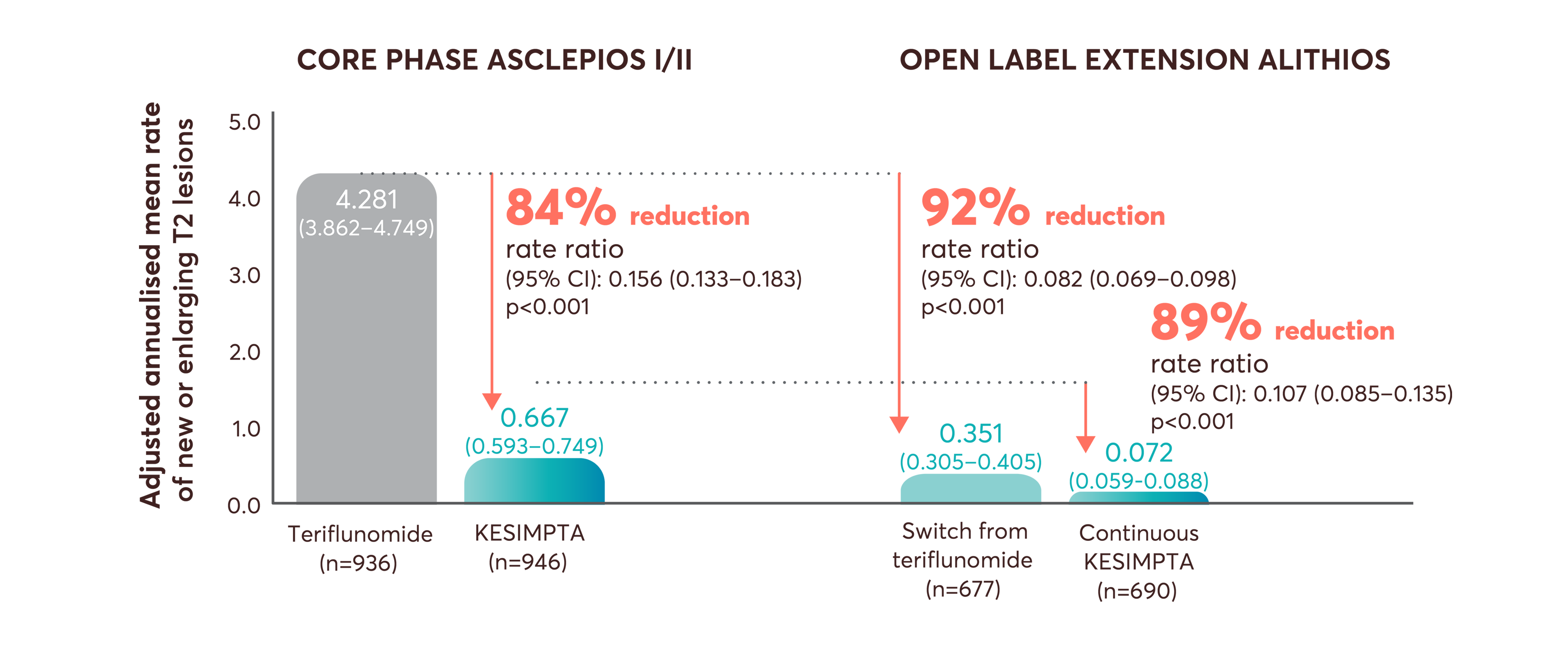
The significant relative reduction in the mean rate of new or enlarging T2 lesions observed for KESIMPTA versus teriflunomide in the core ASCLEPIOS I/II studies was also seen in the extension phase.2
The difference between the switch from teriflunomide group vs continuous KESIMPTA group for the adjusted mean number of T1 lesions (0.013 vs 0.010) during the open-label extension phase was not statistically significant (18% reduction; RR [95% CI]: 0.820 [0.455–1.478]; p=0.509), but a statistically significant difference was seen in the adjusted annualised mean rate of T2 lesions (0.351 vs 0.072; 79.6% reduction; RR [95% CI]: 0.204 [0.159–0.26]; p<0.001).2
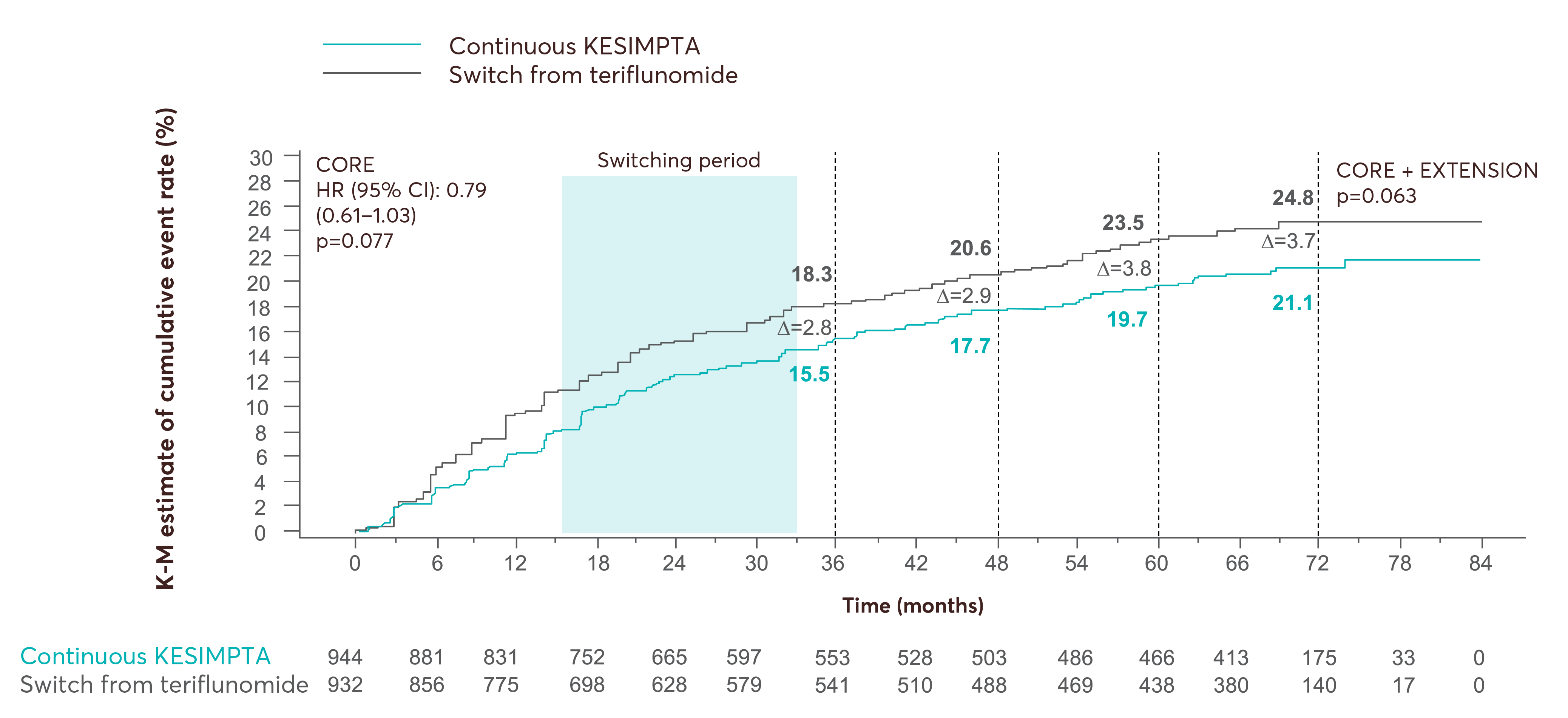
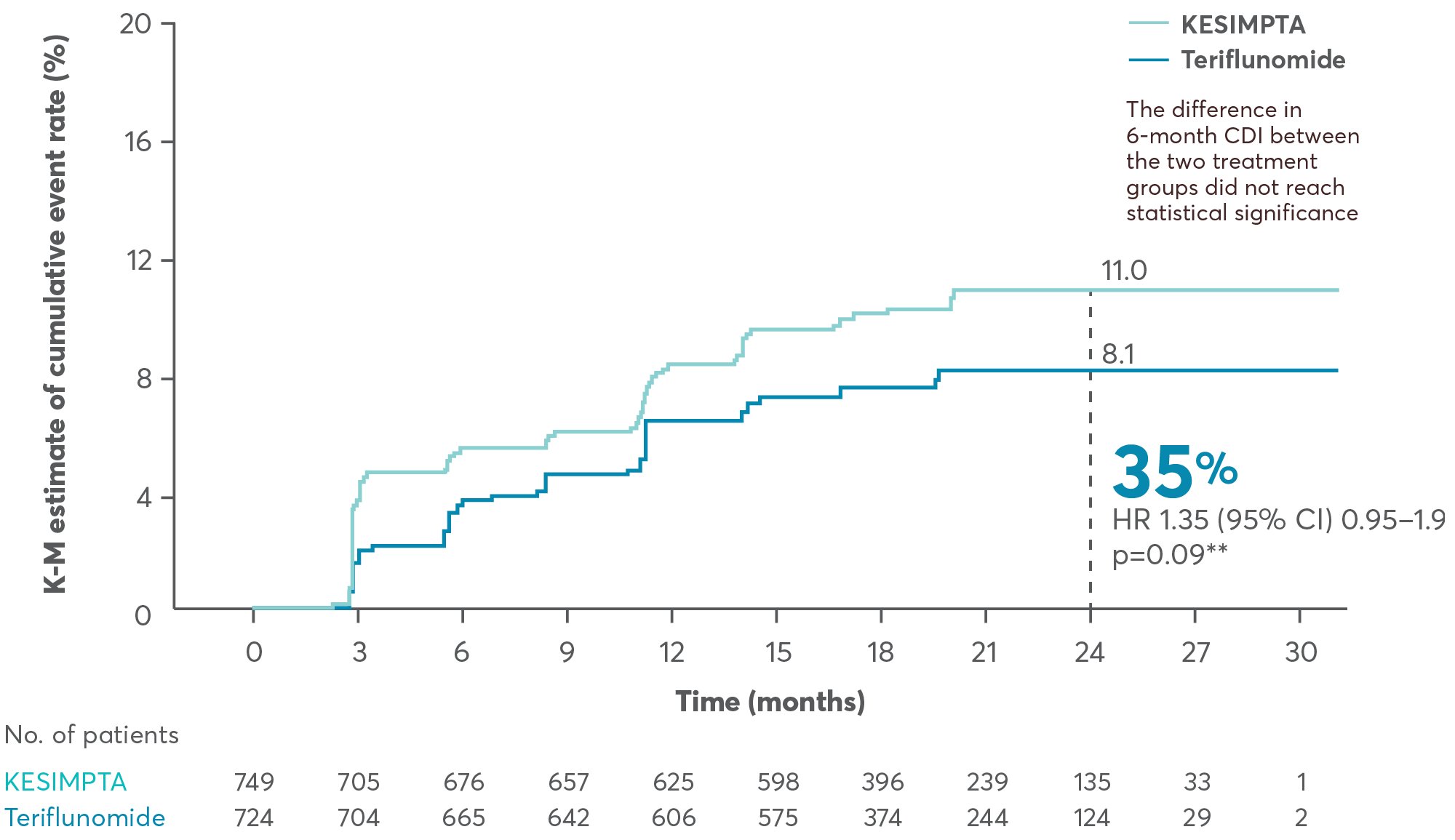
Differences in 6m CDW between continuous and switch group were not statistically significant in the 6-year analysis2
In the ASCLEPIOS I and II trials, the number of patients with confirmed disability worsening at 3 months was 10.9% (n/N=88/944) with KESIMPTA compared to 15% (n/N=125/931) with teriflunomide (HR [95% CI]; 0.66 [0.50–0.86]; p=0.002). At 6 months, it was 8.1% (n/N=71/944) and 12.0% (n/N=99/931), respectively (HR [95% CI]; 0.68 [0.50–0.92]; p=0.01).3
Adapted from Wiendl H, et al. 2024.2
Adapted from Hauser SL, et al. 2019.7
Based on a prespecified pooled analysis of the results of the ASCLEPIOS I and II Phase III pivotal trials for KESIMPTA.7
Adapted from Hauser SL, et al. 2019.7
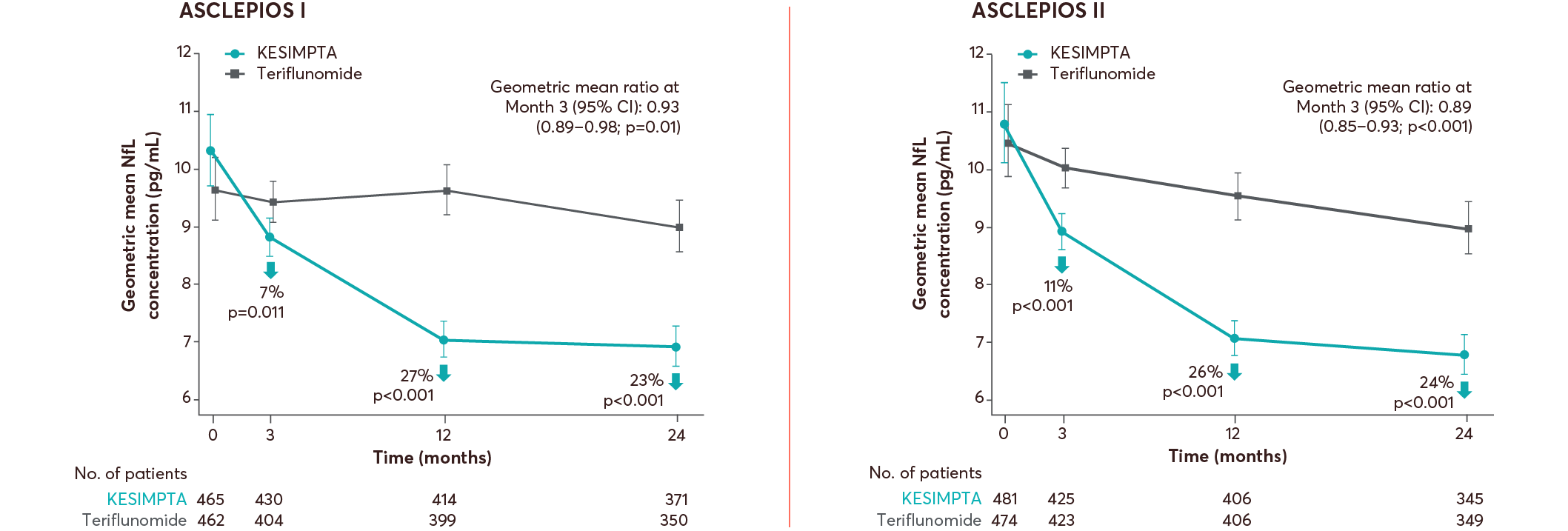
KESIMPTA demonstrated NfL reduction at a 12-month interval of 26–27% across ASCLEPIOS I and II.7
*ARR was defined as the number of confirmed MS relapses per year, according to prespecified criteria. Confirmed relapses are those accompanied by a clinically relevant change in EDSS.3
†ARRs are obtained from fitting a piecewise negative binomial model for the time period core phase and extension phase with log-link, adjusted for treatment and region as factors and number of relapses in previous year, baseline EDSS, baseline number of Gd-enhancing lesions, and the participant’s age at baseline as covariates. The natural log of the time-in-study (in years) by period is used as offset to annualise the relapse rate in each period. Baseline variables are from the core study baseline.2
‡Data from exploratory analyses are descriptive and no confirmatory clinical conclusions can be drawn.
§NEDA-3 is defined as no 6-month confirmed disability worsening, no confirmed MS relapse, no new or enlarging T2 lesions and no T1 Gd-enhancing lesions.2
¶Estimated from fitting a piecewise negative binomial model for the time period core phase and extension phase with log-link, adjusted for treatment as factor and baseline number of T1 Gd+ lesions and participant’s age at baseline as covariates. The natural log of the number of scans with evaluable Gd+ lesion counts by period is used as offset to obtain the lesion rate per scan in each period. Baseline variables are from the core study baseline. All p values are nominal p values.2
‖Analysed via a Cox regression model. 6-month confirmed disability improvement was defined as a decrease from baseline in EDSS score sustained for at least 6 months.3
**Statistical test uses significance (2-sided) level at 0.04875. Cox regression model.7
††ASCLEPIOS I: 7% (8.8 [95% CI: 8.5–9.1] vs 9.4 [95% CI: 9.1–9.8]), 27% (7.0 [95% CI: 6.7–7.3] vs 9.6 [95% CI: 9.2–10.1]), 23% (6.9 [95% CI: 6.6–7.2] vs 9.0 [95% CI: 8.6–9.5]); ASCLEPIOS II: 11% (8.9 [95% CI: 8.6–9.2] vs 10.0 [95% CI: 9.7–10.4]), 26% (7.1 [95% CI: 6.8–7.4] vs 9.5 [95% CI: 9.1–10.0]), 24% (6.8 [95% CI: 6.5–7.1]) vs 9.0 [95% CI: 8.6–9.4]).3
6m CDW, 6-month CDW; ARR, annualised relapse rate; CDI, confirmed disability improvement; CDW, confirmed disability worsening; CI, confidence interval; EDSS, expanded disability status scale; Gd, gadolinium; Gd+, gadolinium enhancing; HR, hazard ratio; K-M, Kaplan–Meier; MS, multiple sclerosis; NEDA-3, no evidence of disease activity-3; NfL, neurofilament light chain; OR, odds ratio; RDTN, recently-diagnosed treatment näive; RR, rate ratio; SmPC, summary of product characteristics.
References
KESIMPTA (ofatumumab) Summary of Product Characteristics.
Wiendl H, et al. Poster P9.010. American Academy of Neurology. 13–18 April 2024, Denver, US.
Hauser SL, et al. New Engl J Med 2020;383(6):546–557.
Hauser SL, et al. Mult Scler 2023;29(11–12):1452–1464.
Cohen JA, et al. Oral presentation 009. American Academy of Neurology. 22–27 April 2023, Boston, MA.
Kappos L, et al. Poster EPR161. European Academy of Neurology. 25–28 June 2022, Vienna, Austria.
Hauser SL, et al. Oral presentation 336. European Committee for Treatment and Research in Multiple Sclerosis, 11–13 September 2019, Stockholm, Sweden.
UK | January 2025 | 443383
Adverse events should be reported. Reporting forms and information can be found at www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Novartis online through the pharmacovigilance intake (PVI) tool at www.novartis.com/report, or alternatively email [email protected] or call 01276 698370.