

This page is intended for UK patients who have been prescribed iptacopan for paroxysmal nocturnal haemoglobinuria.
The information on this website does not replace the patient information leaflet which comes with your medication. Please always refer to your patient information leaflet for more information. If you have any questions, ask your doctor or care team. Connected – Stronger Together is a patient support programme organised and funded by Novartis.
Taking care of your well-being
Setting goals and staying motivated
Connecting personal goals with treatment goals
You might be newly diagnosed with paroxysmal nocturnal haemoglobinuria (PNH) or you may have already received the diagnosis and are switching from a PNH treatment to FABHALTA®▼ (iptacopan).1
Goal setting is important when you’re taking iptacopan, as it will help you stay on track with your treatment and will take you a step towards managing your symptoms.2
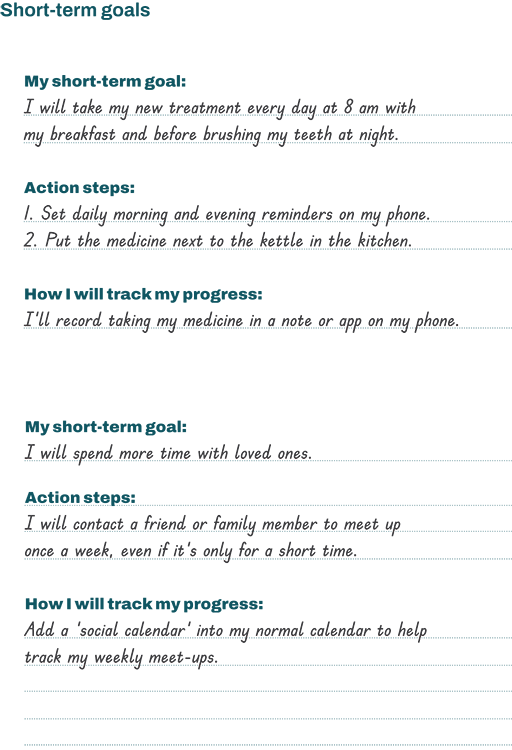
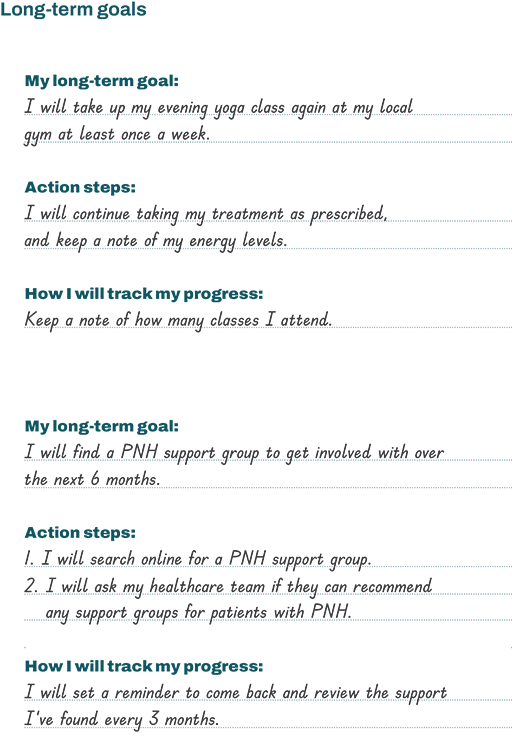
Setting yourself goals can help you achieve the things you care about. They can be short-term (30–90 days), and a stepping stone to your long-term (90 days and beyond) goals.2
For example, a long-term goal could be to contact a PNH support group and get involved over the next 6 months. Short-term steps along the way would be to find out what resources your healthcare team can offer to support you. Another example of a short-term goal is to take your treatment every day at a specific time.
The sample Goal setting planner shows examples of short-term and long-term goals, with space to write down personal goals. You can also find tips on how best to stick to your treatment using mindset and visualisation techniques.
Download the full version of the Goal setting planner, and when you have filled in your goals, share them with your support network.
Download the Goal setting planner
Living well with PNH
Taking care of yourself
Your well-being is a significant factor in the management of your condition. Scheduling time for self-care is an important thing for everyone to do. It’s even more important for people living with a chronic health condition, like PNH. Self-care includes all the activities you do that can help you feel stronger physically and emotionally. That also means hygiene, nutrition and seeking medical care when needed.
As part of your self-care you could do the following:
Prioritise daily activities. Focus on what matters most to you each day. You can save the rest for another day or ask someone else for help with it
Take care of yourself. Getting enough sleep, eating well and taking light exercise each day are all important. Do what you can, when you can, and forgive yourself when you can’t
Reframe your ‘cannots’. Instead of saying, ‘I cannot go through all these emails,’ try saying, ‘I can answer three important emails today and save the rest for later’
The Making time for self-care guide contains more tips on how to take care of your well-being. It also contains a calendar in which you can write down activities that can form part of a self-care routine.
Download the Making time for self-care guide
One of the most common symptoms of PNH is fatigue due to anaemia. People who don’t experience fatigue may not understand that it’s different from just feeling tired. It’s a long-lasting exhaustion that isn’t relieved by getting rest.3–5
You may have experienced how fatigue can reduce your energy, motivation and concentration. However, there are still things you need to do day to day, like chores and other tasks. It’s hard to do those things when you feel exhausted.
By balancing rest and activity, you can help reduce your symptoms or avoid making them worse. Planning ahead can help you use the energy you have wisely, based on what your body is telling you each day.
Here are some tips to manage fatigue:6,7
Set yourself a routine. By following a routine, you can manage your energy so that you can do your daily activities. People have different routines, so follow a routine that suits you
When it comes to housekeeping, store the items you use most often in a place where you can get them easily, without reaching or going up and down stairs (for example, keep paper towels on the kitchen counter)
Use your phone or a planner to organise appointments so that you can avoid scheduling them too close together
Break down chores into smaller steps – for instance, plan to clean a couple of rooms a day rather than the whole house
Ask for flexible work arrangements, like travelling to and from work at less busy times, if you can
When possible, use electric appliances, like a dishwasher, mixer, or food processor, so you don’t have to do these tasks by hand
Sit down when you’re doing basic activities, like dressing, folding laundry, ironing, or outdoor work
You can also be proactive about managing your energy levels throughout the day. Here are some tips to help you with this:
Prioritise daily activities. Put what is most important each day at the top of your list and leave the rest for another day
Ask others to help you. Give a ‘heavy duty’ activity, like vacuuming or washing your bedding, to other people in your support network
Plan for rest. Schedule regular rest periods or ‘down time’ in your day. For example, take short naps after lunch at the weekend or 10-minute breaks throughout the working day
Be kind to yourself. Some days you may feel more fatigued than others. Give yourself a chance to listen to your body and take it easy that day
The Making time for self-care guide gives you further tips on how to manage your fatigue and energy levels, as well as other tools to help with your self-care.
Download the Making time for self-care guide
Sleep is just as important for good health as fatigue management. Getting enough sleep is essential to staying healthy, especially when living with a chronic condition like PNH. Adopting good sleep habits can help you feel rested and boost your overall well-being.8,9
Here are some tips for getting a good night’s sleep:10
Try to create a relaxing bedtime routine
Keep your bedroom cool and dark at night
Try to go to bed at the same time every night
Avoid using electronic devices before bedtime, such as TV, video game consoles, or your mobile phone or tablet. The blue light these give off may make you feel more alert. If you keep your phone near your bed, put it on silent
Avoid caffeine, alcohol, and high-sugar foods several hours before bedtime
In the Making time for self-care guide you can find a sleep diary in which you can record the length and quality of your sleep on a daily basis. This can help you decide what adjustments to make to get a good night’s sleep.
Download the Making time for self-care guide
Sometimes we think of habits as things that we need to change. But there are healthy habits, like having a good sleep routine, brushing our teeth, and keeping fit, which may help manage your condition.
The thought of exercising may seem overwhelming, especially when PNH can make you feel fatigued. However, light exercise such as walking, stretching, or riding a stationary bike may actually help fatigue by:11
Increasing your energy levels
Increasing your strength
Improving your ability to do everyday tasks
Improving your sleep
Before starting any exercise or physical activity routine, it’s important to talk with your doctor to make sure it’s okay to do so. A good approach to doing exercise is to start slowly, working towards a balance between rest and exercise. Listen to your body, and rest when you need to.
Download the Making time for self-care guide
The benefits of good nutrition and healthy eating can’t be underestimated. Food really is the fuel of our bodies, and what we put into them matters. Fuelling your body with healthy foods can help you manage the fatigue caused by PNH and provide other benefits too. It’s not easy to eat healthily all the time, but there are some things you can do to make it easier:12–14
Include a variety of fruit and vegetables, whole grains and legumes12,13
When it comes to animal proteins, prioritise fish, lean meats, and poultry, as well as low-fat dairy foods13
Limit the amount of red or processed meats and other highly processed foods13
Stay hydrated. If you don’t drink enough water you may get dehydrated, which means you lose more fluid from your body than you take in. Ask your doctor how much water or fluids they recommend for you each day to help you stay hydrated13
Keep snacks on hand. This may help when you feel your energy is low, if you have an upset stomach or need a quick meal. Crackers or grain bars are easy snacks you can take with you13
Eating healthily is a form of self-care and can feel rewarding when you get into the habit of making your self-care a priority. Remember to reward yourself for making healthy choices. The Making time for self-care guide contains tips on ways you can reward yourself.
Download the Making time for self-care guide
Overcoming difficult emotions
Understanding your feelings
Many people experience difficult emotions that come with a chronic condition like PNH. For some patients it takes years to reach a diagnosis, which can be stressful. Once you’ve been diagnosed, you may feel the fear and uncertainty that can come with having a rare condition. This can be overwhelming and raises a lot of emotions.
Your emotions may affect you in other ways. If you have low mood you may experience:
A change in weight (gaining or losing weight)
Chronic pain or inflammation
Sexual health problems
Trouble sleeping
Stomach pains and digestive problems
You may experience negative or gloomy thoughts. Such thoughts might be:
Always expecting the worst
Only focusing on what makes you feel bad
Seeing things as only good or only bad
Blaming yourself for negative situations
That’s normal. It’s hard to be optimistic all the time. These unhelpful thoughts can make you feel anxious and affect your mental health and well-being. When you start to have these thoughts, it helps to adopt a technique called ‘reframing’.
Reframing is when you take a step back and ask yourself – what are the actual facts? Then look for other ways to see the situation.2,15,16
For example, you have an important task to do at work, and you’re worried you’ll fail at it. This then makes you feel worse. Instead of believing this, catch the thought and take a moment and ask yourself a few questions:16
How likely is this to happen?
Is there good evidence for it?
Are there other possible outcomes?
Is there good evidence for alternative ways of looking at the situation?
What would you say to a friend if they were thinking this way?
Tips for reframing and managing your thoughts
Be kind to yourself. If you start having unhelpful thoughts, speak to yourself in the same kind way you’d speak to someone you love
Keep practising. It takes awareness and effort to reframe unhelpful thoughts, but it can be done over time
Note down your feelings such as anxiety, sadness, anger, or stress, and try to recognise any patterns or triggers for these types of feelings
Write your feelings down in a journal. This is a great way to express yourself, get feelings off your chest, and help you better examine your thoughts. You can download the Treatment diary and use this to record your emotions
Share your notes and thoughts with your healthcare team
Practise positive self-talk. Write down a few phrases that start with the words ‘I am’ or ‘I will’. For example ‘I am able to do this’ or ‘I will get through this’2,17
Self-care is a very useful habit to adopt. As little as 10 minutes of self-care can help reduce negative emotions.
Examples of self-care are:
Doing something that lowers stress, like yoga
Taking a relaxing warm bath
Listening to your favourite music
Getting some light exercise
Calling a friend
When you feel stressed or have anxious thoughts, your body can tense up. Many people find that slowing down their breathing helps. Sit or lie in a comfortable spot and try this simple slowed breathing exercise for a full minute:
Count to 4 (1-2-3-4) as you take a slow, deep breath in, and count to 4 (1-2-3-4) again as you hold it, and finally, count to 4 (1-2-3-4) as you slowly release the breath
Repeat for a full minute
Notice any physical changes in your body, such as a slowed heart rate or less muscle tension
Notice if you feel a sense of calm
Download the Treatment diary
When to contact your healthcare team
There are a lot of coping strategies you can use to help manage your emotions or low mood. If any of these emotions – like sadness, anger, or anxiety – last for a long time or interfere with your everyday life, it’s important that you talk to your healthcare team, who can arrange additional help.
Download the Caring for your emotional health leaflet
Seeking support
Remember, you’re not alone and support is available. It’s important to know what kind of support there is and where you can get it. Support can be social, practical, emotional or informational.18,19
Social support
In addition to your healthcare team, your network of friends, family, or other people close to you form the bedrock of your social support. They are people you can turn to when you’re faced with a challenge, like living with a chronic condition.18,20
Tips for getting social support:
Rely on your healthcare team. They won’t find it a burden to help you. They want to help you! Ask your questions, and share your challenges and successes so they can support you
Practise asking others for help. Think about how you might fill in these blanks. ‘[Person’s name], can you please help me with [chore or task] on [specific date/time]?’
Connect with support groups. Hearing from other people who are navigating daily life with PNH can offer you comfort and wisdom
Practical support
This means tangible help and services. This can be childcare for your kids, picking up your medicine from the pharmacy, help with household chores, running errands, preparing meals, or providing transportation to get to an appointment.19
Needing practical support is nothing to feel guilty about. You’re not letting anyone down if you ask for help when you’re not feeling well.
Think about who you’d ask for help with a specific task and what steps you’d take to get that support. For example, you may decide to ask a member of your support network to drive you to your next medical appointment.
Tips for getting social support:20
Identify people in your network. Make a list of people in your life who could help you
Write down your own practical needs. Think about what practical tasks and activities you’ll need help with
Match names with tasks. Link the best person to help you with a particular task and note down how you’d ask them for support
Emotional support
Empathy, care, love, and trust are the main aspects of emotional support. When we receive this kind of support, we feel validated and accepted. Emotional support can be very helpful when you’re feeling down about things, like missing out on social activities or hobbies you enjoy because you’re too tired to do them.18,20
Emotional support can come from your healthcare team or a support group.
Tips for getting emotional support:
Find a good listener. Emotional support makes you feel less lonely and better understood. Think of people in your life who are good listeners. Note down the words you’d use to let them know that you’re not feeling good and you need to talk. For example, you could say, ‘Can we talk after dinner? You don’t have to do anything but listen’
Talk with your healthcare team. Tell them how you’re feeling, especially if it’s a difficult emotion that doesn’t go away or gets in the way of your everyday life. They can then provide appropriate resources to help you
Informational support
This includes advice, suggestions, or information you need to have the knowledge on your condition. Having the facts can help you understand how PNH affects you and why you need to stay on treatment to manage it.18
Your doctor and other members of your healthcare team can provide you with the informational support you need. For example, this can be someone on your healthcare team taking time to explain test results so that you can better understand the information. You can also look to The National PNH Service and other local or regional organisations, as well as patient support groups for general information about PNH, and more resources for patients and caregivers.
Tips for getting informational support
Work out what you don’t understand. If there’s something you’re unclear on regarding your treatment or your condition, write down a list of questions you have on that subject
Call your healthcare team if you need urgent support. Otherwise, if there is no urgency, keep a running list of questions to take to your next appointment
Ask your healthcare team questions. Use your list to ask for help in understanding, for example, why you need to take a booster vaccine
If the information you’re getting during your visit isn’t communicated clearly, you can:
Ask the healthcare team to write it down for you
Repeat back what the healthcare team has said in your own words to check your understanding – for example, ‘What you said is sticking to the prescribed dose of my medication reduces the risk of red blood cells being broken down. Is that right?’
How to find support groups
Many people find it helpful to share experiences with other people living with PNH. Although everyone’s treatment path and PNH experience is unique, talking with someone who has shared a similar experience may provide comfort and make you feel less alone.
One thing you can do to find support is ask your healthcare team about support services and support groups available.
Resources and FAQs
Here you can download tools that can help you manage your treatment and condition, as well as find answers to questions you may have about iptacopan or PNH. There is also information on local support groups and websites.
Resources and FAQs
References
FABHALTA® Package Leaflet – Information for the patient.
Michie S, et al. Ann Behav Med 2013;46(1):81–95.
PNH Support. Signs and symptoms. Available at: https://pnhuk.org/what-is-pnh/signs-and-symptoms/#:~:text=PNH%20patients%20experience%20differing%20levels,the%20haemoglobin%20levels%20are%20normal. [Accessed October 2024].
Brodsky RA. Blood 2014;124:2804–2811.
Mayo Clinic. Fatigue. Available at: https://www.mayoclinic.org/symptoms/fatigue/basics/definition/sym-20050894. [Accessed October 2024].
Vatwani A & Margonis R. Arch Phys Med Rehabil 2019;100(6):1193–1196.
Ray TK & Pana-Cryan R. Int J Environ Res Public Health 2021;18:3254.
Buysse DJ. Sleep 2014;37(1):9–17.
Centers for Disease Control and Prevention. Sleep and Sleep disorders. How Much Sleep Do I Need? Available at: https://www.cdc.gov/sleep/about/?CDC_AAref_Val=https://www.cdc.gov/sleep/about_sleep/how_much_sleep.html. [Accessed October 2024].
The Leukemia & Lymphoma Society® (LLS). Cancer-related fatigue. Available at: https://lls.org/treatment/managing-side-effects/cancer-related-fatigue. [Accessed October 2024].
Memorial Sloan Kettering Cancer Center. Managing Cancer-Related Fatigue. Available at: https://www.mskcc.org/cancer-care/patient-education/managing-related-fatigue. [Accessed October 2024].
The Leukemia & Lymphoma Society® (LLS). Food and Nutrition. Available at: https://www.lls.org/managing-your-cancer/food-and-nutrition. [Accessed October 2024].
American Cancer Society. Nutrition for the Person With Cancer During Treatment. Available at: https://www.cancer.org/content/dam/cancer-org/cancer-control/en/booklets-flyers/nutrition-for-the-patient-with-cancer-during-treatment.pdf. [Accessed October 2024].
Gropper SS. Nutrients 2023;15:664.
D’Arbeloff TC, et al. Emotion 2018;18(6):912–915.
NHS UK. Better Health. Every Mind Matters. Reframing Unhelpful Thoughts. Available at: https://www.nhs.uk/every-mind-matters/mental-well-being-tips/self-help-cbt-techniques/reframing-unhelpful-thoughts/. [Accessed October 2024].
Hamilton R, et al. Curr Oncol 2011;18(2):e46–53.
Sam N, M.S. Psychology Dictionary Professional Reference. 2023. Social Support. Available at: https://psychologydictionary.org/social-support/. [Accessed October 2024].
Sheurer D & Choudry N. Am J Manag Care 2012;18(12):e461–e467.
American Psychological Association. Manage Stress: Strengthen Your Support Network. Available at: https://www.apa.org/topics/stress/manage-social-support. [Accessed October 2024].
UK | October 2024 | FA-11228108
Reporting side-effects
If you get side-effects with any medication you are taking, talk to your doctor, pharmacist or nurse. This includes any possible side-effects not listed in the information leaflet that comes in the pack. ▼ The medicine referred to in this material is subject to additional monitoring. This will allow quick identification of new safety information. You can help by reporting any side-effects you may get. Please see www.mhra.gov.uk/yellowcard. for instructions on how to report side-effects.
Reporting side-effects
If you get side-effects with any medication you are taking, talk to your doctor, pharmacist or nurse. This includes any possible side-effects not listed in the information leaflet that comes in the pack. You can report side-effects via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard.
By reporting side-effects you can help provide more information on the safety of your medication.